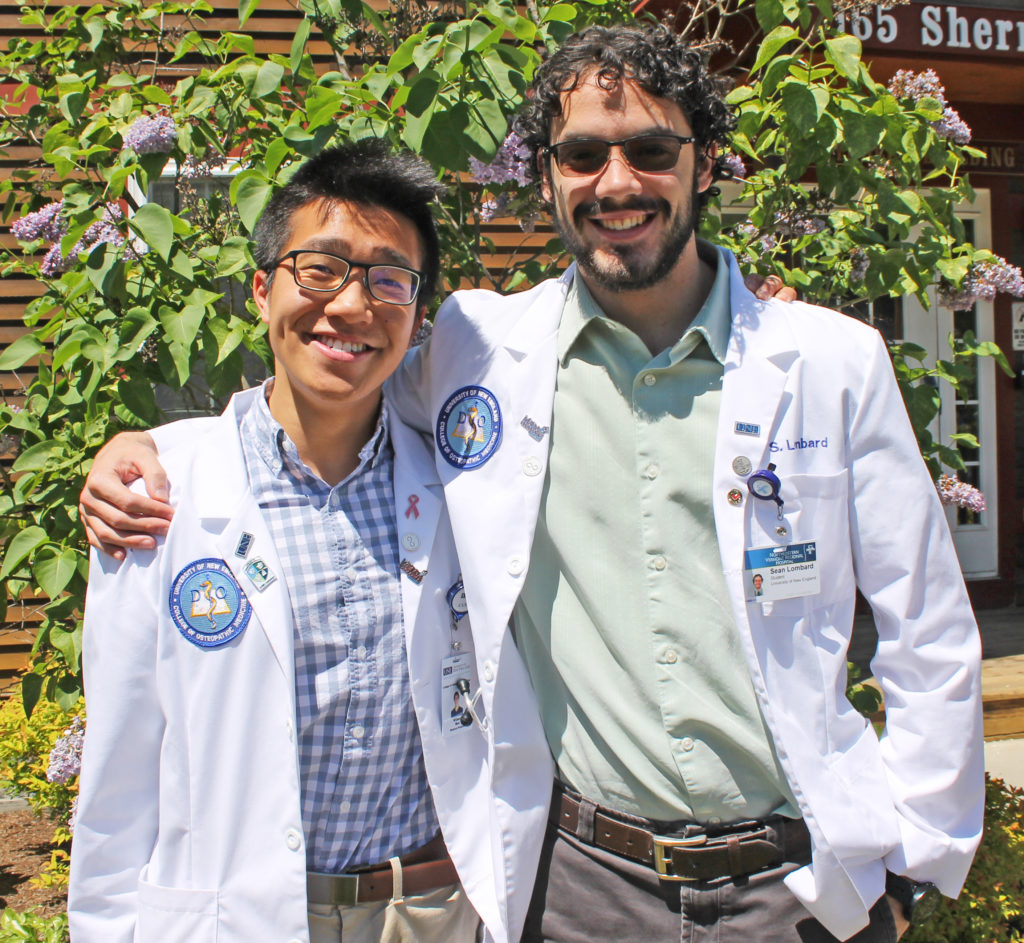
Students Sean Lombard and Wilson Mei, who have both recently finished their first year of medical school at the University of New England (UNE), completed a one month pilot immersion program at Northeastern Vermont Regional Hospital (NVRH) and Northern Counties Health Care on June 7, 2019. This immersion program, which is the first to run in Vermont’s Northeast Kingdom for UNE’s College of Osteopathic Medicine, is intended to introduce and highlight patient-centered care early on in a medical student’s education.
“It’s a great way to start early in training to understand what options lie ahead for the future,” said Dr. Victoria Thieme, DO, Director of Clinical Experience for UNE Osteopathic Medicine.
Three years ago, Laura Newell, VP of Medical Practices at NVRH, met with Christopher Towne, Director of Federally Qualified Health Centers (FQHC) Operations at Northern Counties Health Care, Inc. and Dr. Thieme to establish a way for UNE students to get more clinical experience early in their medical school training. This experience not only introduces students to different specialties and methods of practicing medicine, it highlights the importance and value of practicing in Vermont’s rural and underserved communities.
There is also a research component. Lombard worked with Dr. Thieme to design a project that would look at how individuals with substance abuse disorders are tracked. Vermont’s system of Medication Assisted Treatment is through the Hub and Spoke model, which supports people in recovery from opioid use disorder by offering “hubs,” locations that offer daily support, and “spokes,” supports set up within general healthcare services. Lombard, Mei and a third student who participated in an immersion program in Maine, which does not have a Hub and Spoke model, gathered data and plan to compare outcomes.
The focus of UNE’s immersion program is to expand student interest through shadowing, potentially connecting new-found interests with rural healthcare needs.
“I had immediately ruled out psychiatry and family medicine,” said Mei. “But having shadowed in family medicine and psychiatry, I realize I was entirely wrong about my perception of these fields. Being exposed to all these different departments, I got to see a wide range of what it means to be a rural physician. Going into 2nd, 3rd and 4th year, I’ll be more open minded.”
“You see people who are really good at what they do,” said Lombard. “And you want to be like that.”
Press Release courtesy of Northern Vermont Regional Hospital